Colon Polyps Introduction
A polyp, which can be flat, raised or on a stalk, is a growth in the large intestine or rectum. You may not have symptoms, so screening is needed to help prevent a polyp turning into colorectal cancer. Screening methods include colonoscopy, sigmoidoscopy, a stool test or a CT scan.
What are colon polyps?
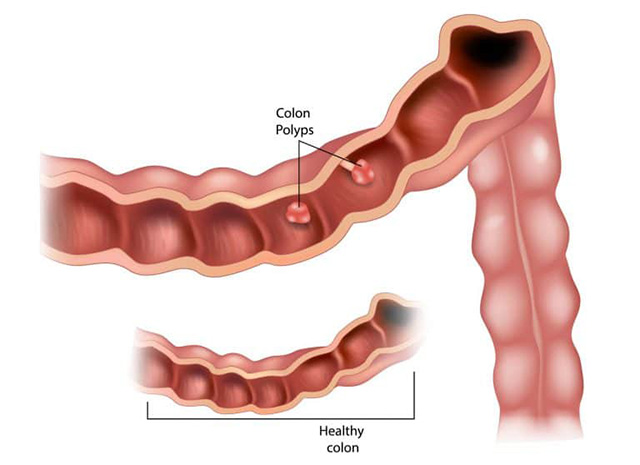
A colon polyp is a growth on the inner lining of the colon (large intestine) or rectum. A polyp can have a variety of shapes and be flat, slightly raised (called sessile) or on a stalk (called pedunculated). There are different microscopic types of polyps (which require a microscope to determine), and the adenomas or sessile serrated polyps can eventually grow over time and become cancer. Undergoing colorectal cancer screening and removal of polyps can decrease the risk of developing colorectal cancer.
What causes colon polyps and who gets them?
Polyps are found in about 30% of the adult population over the age of 45-50. Men and women of all ethnicities are at risk of colon polyps and colon cancer.
A polyp is the result of genetic changes in the cells of the colon lining that affect the normal cell life cycle. Many factors can increase the risk or rate of these changes. Factors are related to your diet, lifestyle, older age, gender and genetics or hereditary issues. Important lifestyle factors predisposing to colorectal polyps and cancer (making you more liable to get these conditions) include:
Smoking.
Excess alcohol ingestion (drinking too much alcohol).
Not exercising.
Being overweight.
Eating processed foods and too much red meat (instead of a mostly plant-based food plan).
Other factors include:
Having a personal history of colorectal polyps or colorectal cancer.
Having a personal history of inflammatory bowel disease (Crohn's disease or ulcerative colitis) or primary sclerosis cholangitis.
What are the symptoms of colon polyps?
Most colon polyps and early, curable colorectal cancer do not have any symptoms, which is why screening is recommended. However, when symptoms do occur, they may include:
Bleeding from the rectum (the last part of the digestive tract that enables stool to leave the body), which can be seen with the naked eye or detected microscopically by fecal blood test or a fecal blood test combined with a genetic stool test.
Unexplained iron deficiency anemia or weight loss.
Change in normal bowel movement pattern.
Abdominal pain (rare).
The above symptoms should be evaluated to ensure that there are no polyps or colorectal cancer.
How are colon polyps diagnosed?
A doctor can find colon polyps in several different ways, including:
Colonoscopy: A procedure in which a long, thin, flexible tube is placed through the rectum and into the large intestine. The tube has a camera that shows images on a screen and allows polyps to be removed.
Sigmoidoscopy: A thin, flexible tube is inserted through the rectum to examine the last third of the large intestine (sigmoid colon).
Computerized tomography (CT) scan: A radiology test that uses radiation to create pictures of the large intestine.
Stool tests: You provide the lab with a stool sample, which will be tested for blood or genetic changes suggestive of polyps and cancer. If the test is positive, a colonoscopy is needed.
If any of the last tests are abnormal, a colonoscopy should be done to check for polyps and remove them.
What happens if you have a colon polyp?
When a colon polyp is found, your doctor will remove it (polypectomy) and test it in the laboratory to see what microscopic type it is (biopsy). Your doctor will determine when you should have a repeat screening test based on the number, size and microscopic analysis of polyps, in addition to your other risk factors.


 Doctor Messenger Consultation
Doctor Messenger Consultation